Eating Disorders Explained: From Triggers to Symptoms
What is an Eating Disorder (ED)?Types of eating Disorders (ED)?Anorexia Nervosa Binge Eating Disorder Bulimia Nervosa Orthorexia Nervosa Why do people develop an eating disorder? The Body’s Biochemistry Genetics Environment Culture How to treat an Eating Disorder?
Let’s explore the world of eating disorders, including anorexia nervosa, Orthorexia Nervosa, bulimia nervosa, and binge eating disorder. Understand the causes, symptoms, and recovery journeys. Delve into the impact of body image, emotional eating, and media influences. Discover key statistics and prevention strategies for these complex conditions.
What is an Eating Disorder (ED)?
Eating disorders involve three main aspects: physical, mental, and spiritual. Physically, they can be seen through a person’s eating habits, whether it’s excessive eating or strict control. Mentally, there is an unhealthy obsession with food and controlling eating, which can harm the body. Spiritually, the person may feel empty and disconnected, and their relationships may suffer. These disorders can also lead to serious health problems like diabetes or heart disease. In essence, the joy and vitality in life are replaced by suffering. The solution lies in recognizing the problem and seeking treatment and recovery, just like a diabetic needs regular medication.
Types of eating Disorders (ED)?
Eating disorders distort the natural act of eating through patterns of overeating or strict control. In this section, we will explore four types of eating disorders, three of which are recognized by the DSM-V diagnostic manual. These disorders include:
Anorexia Nervosa
Anorexia Nervosa is a condition where individuals deliberately limit their food intake due to a fear of gaining weight. Those affected, often young girls and homosexual men, avoid meals in their pursuit of remaining thin or slim. This disorder is closely linked to body-image concerns and Pocrescophobia, which is the fear of becoming fat.It is recognized as an approved illness and can be diagnosed using the DSM-V criteria.
Here are some common symptoms associated with Anorexia:
- Significant weight loss: Rapid and drastic weight loss, often resulting in being significantly underweight for one’s age, height, and body type.
- Restriction of food intake: A persistent restriction of calorie intake, leading to an extremely limited and restrictive diet. This may involve avoiding certain types of food, food groups, or specific macronutrients.
- Distorted body image: A distorted perception of one’s body and an intense fear of gaining weight or becoming overweight, despite being underweight.
- Excessive exercise: Engaging in excessive and compulsive exercise routines, often driven by the need to burn calories and control weight.
- Rituals and food-related behaviors: The development of strict rituals and behaviors around food, such as cutting food into small pieces, rearranging food on the plate, or avoiding eating in public.
- Obsessive thoughts about food and weight: Constant preoccupation with thoughts about food, weight, and body shape, which may interfere with daily activities and relationships.
- Social withdrawal and isolation: Withdrawing from social activities and isolating oneself due to the preoccupation with food, weight, and body image concerns.
- Physical complications: Anorexia can lead to various physical complications, including fatigue, dizziness, fainting, low blood pressure, electrolyte imbalances, hair loss, brittle nails, constipation, and disruptions in menstrual cycles in females.
Binge Eating Disorder
Binge Eating Disorder (BED) is a condition characterized by recurrent episodes of uncontrollable and excessive food consumption, where individuals feel unable to exert control over their eating behaviors. Unlike food addiction, BED does not involve a loss of control. If left untreated, this disorder can have serious health implications, including the increased risk of developing conditions such as diabetes, heart disease, and various types of cancer. It is important to seek BED treatment immediately after it is recognized to prevent further health complications and promote overall well-being.
Here are some common symptoms associated with BED:
- Frequent episodes of binge eating: Eating large amounts of food in a short period, typically within a two-hour timeframe, without feeling hungry or physically satisfied.
- Loss of control: A sense of being unable to stop or control the amount of food being consumed during binge episodes.
- Rapid eating: Eating quickly during binge episodes, often to the point of discomfort or pain.
- Eating beyond fullness: Continuing to eat even when feeling physically full or uncomfortably stuffed.
- Eating alone or in secret: Feeling embarrassed or ashamed about the binge eating behavior, leading to consuming food in private or hiding evidence of binge episodes.
- Distress and emotional impact: Experiencing feelings of guilt, shame, or disgust following binge eating episodes, which can contribute to emotional distress and negative self-perception.
- Absence of compensatory behaviors: Unlike Bulimia, individuals with BED do not regularly engage in compensatory behaviors such as vomiting, excessive exercise, or strict dieting after binge episodes.
- Weight fluctuations: Fluctuations in weight, often leading to overweight or obesity, as a result of the recurrent binge eating episodes.
Bulimia Nervosa
Bulimia Nervosa is characterized by consuming large quantities of food, similar to those experiencing Binge Eating Disorder (BED). However, unlike BED, bulimia is accompanied by purging behaviors. Purging may involve intentional vomiting or excessive exercising. This process is often conducted in secrecy due to the shame associated with it. It is recognized as an approved illness and can be diagnosed using the criteria outlined in the DSM-V.
Bulimia Nervosa is characterized by a pattern of recurrent episodes of binge eating, followed by compensatory behaviors to prevent weight gain. Here are some common symptoms associated with Bulimia:
- Binge eating: Frequent episodes of consuming large amounts of food within a discrete period, often accompanied by a loss of control over eating during these episodes.
- Compensatory behaviors: Engaging in behaviors to compensate for the calories consumed during binge eating episodes, such as self-induced vomiting, excessive exercise, fasting, or misuse of laxatives or diuretics.
- Preoccupation with body shape and weight: An intense concern with body shape, weight, and self-image, with a strong desire to achieve and maintain a specific, often unrealistic, body weight or shape.
- Frequent dieting or restrictive eating: Consistent efforts to restrict food intake or follow strict diets, which may alternate with episodes of binge eating.
- Secretive behavior: Hiding or being secretive about eating habits, including binge eating and purging behaviors, due to feelings of shame, guilt, or embarrassment.
- Dental problems: Frequent exposure of teeth to stomach acid from vomiting can lead to tooth decay, erosion of tooth enamel, and other dental issues.
- Physical complications: Bulimia can result in various physical complications, such as gastrointestinal problems, dehydration, electrolyte imbalances, irregular menstrual periods, chronic sore throat, swollen salivary glands, and fluctuations in weight.
- Emotional distress: Individuals with bulimia often experience feelings of guilt, shame, low self-esteem, and depression related to their eating behaviors.
Orthorexia Nervosa
ON is characterised by nutritional obsession at the expense of enjoying one’s meal. Its sufferers are afraid of eating the wrong thing for fear of illnesses related to nutritional problems. ON is listed under EDNOS (Eating Disorders Not Otherwise Specified). In the DSM-V, those suffering from ON will get an EDNOS diagnoses because it does not fall into the category of BED, AN, or BN.
Here are some common symptoms associated with Orthorexia:
- Obsession with healthy eating: An extreme preoccupation with consuming only foods that are deemed “clean,” “pure,” or considered healthy according to specific criteria or dietary rules.
- Strict dietary restrictions: Imposing strict rules and restrictions around food choices, often eliminating entire food groups or demonizing certain foods perceived as unhealthy or impure.
- Anxiety and distress related to food: Experiencing significant anxiety, guilt, or distress when faced with foods that are outside the self-imposed dietary rules or restrictions.
- Social isolation and withdrawal: Avoiding social situations involving food, such as gatherings or meals with friends or family, due to the fear of not being able to adhere to strict dietary requirements.
- Declining quality of life: A diminished quality of life due to the constant focus on food and the impact of dietary restrictions on everyday activities, relationships, and overall well-being.
- Negative impact on mental health: Developing obsessive and rigid thinking patterns related to food, body image, and self-worth, which may lead to increased anxiety, depression, or even orthorexic-related compulsive behaviors.
- Nutritional deficiencies: Over time, strict dietary restrictions may result in inadequate nutrient intake and nutritional imbalances, leading to physical health problems and compromised well-being.
Why do people develop an eating disorder?
As previously mentioned, it is crucial to understand that having an eating disorder is not a conscious decision made by individuals, it is identified as an addiction Therefore, it is not their fault that they have developed this disease. In the same way, one cannot blame someone with asthma or diabetes for their condition. It is essential to avoid self-blame if you are experiencing an eating disorder. However, it is important to take responsibility for your recovery moving forward. Exploring the reasons for developing an eating disorder can help shed light on its complex nature. Here are some factors that can contribute to the development of an eating disorder:
The Body’s Biochemistry
Individuals with Binge Eating Disorder (BED) often have imbalances in neurotransmitters like serotonin and cortisol. This leads to high stress and low pleasure. To compensate, they may turn to food to trigger the release of dopamine, the pleasure neurotransmitter.
Genetics
Individuals with eating disorders often have a familial history of the illness. Parents who utilize food as a coping mechanism to soothe their emotions may pass on this pattern to their children through genetic factors. Certain chromosomes have been identified as being associated with a higher susceptibility to Bulimia and Anorexia. Additionally, twins are more prone to developing eating disorders compared to non-identical siblings.
Psychologically, individuals with eating disorders commonly experience co-occurring mental illnesses such as depression, obsessive-compulsive disorder, and anxiety disorders. These comorbid conditions contribute to distorted thinking patterns and beliefs. Examples include perfectionism, low self-esteem, impulsivity, and difficulty expressing emotions. These psychological factors play a significant role in the development and maintenance of eating disorders.
It is important to recognize the multifaceted nature of eating disorders, involving both genetic and psychological influences. By understanding these factors, we can gain insight into the complexity of these illnesses and the various elements that contribute to their onset and progression.
Environment
The development of eating disorders is influenced by a combination of the sufferer’s past and present circumstances. In some cases, individuals with eating disorders may have a history of experiencing sexual or physical abuse, which can contribute to their struggles. Some more factors that contribute to EDs are:
- Diet culture
- The media
- Trauma
- Weight teasing
Additionally, underlying childhood trauma or challenging family relationships may play a significant role in the onset of these disorders. Exploring the connection between childhood trauma and the development of addiction can provide further insights into the complex interplay of factors.
Culture
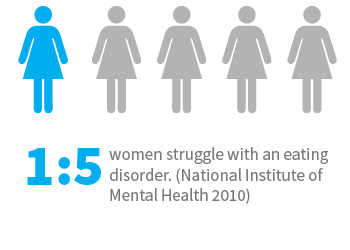
The influence of culture on eating disorders, such as Anorexia, Bulimia, Orthorexia, and Binge Eating Disorder (BED), is significant and multi-faceted.
- Cultural emphasis on achieving a slim and beautiful physique serves as a potent catalyst for the development of disorders like Anorexia and Bulimia. Society’s pervasive message
- Society equating thinness with beauty can fuel an individual’s desire to conform to these ideals, leading to disordered eating patterns.
- The pursuit of healthy eating, which initially starts with good intentions, can sometimes evolve into Orthorexia
- Cultural norms, including media representations and societal pressures, can shape these perceptions of what constitutes healthy eating, further contributing to the development of Orthorexia.
- The prevalence of unhealthy foods in the market poses a challenge for individuals with BED who strive to maintain food sobriety.
- The association of certain foods, particularly sugary or indulgent treats, with love and celebration across various cultures adds to the complexity. These cultural associations can trigger emotional connections to food, making it difficult for BED sufferers to resist the urge to engage in binge eating behaviors.
Overall, culture plays a significant role not only in triggering the onset of eating disorders but also in perpetuating and maintaining them. Awareness of these cultural influences is vital for understanding the complex interplay between societal expectations, food norms, body image ideals, and the development and perpetuation of eating disorders.
How to treat an Eating Disorder?
In order to effectively treat an eating disorder, it is crucial to recognize it as a genuine illness. Without intervention, untreated eating disorders cannot resolve on their own. Whether it involves controlling or overeating, food becomes an unmanageable aspect of the individual’s life. Acknowledging this powerlessness over food is a vital step in the recovery process. Seeking guidance from a qualified nutritional clinician can assist in making informed choices regarding food.
It is important to note that eating disorders fall under the category of process addictions. Unlike substances, complete abstinence from food is not possible as it is an essential part of daily life. Therefore, a balanced dietary approach that includes meal planning and nutritional advice becomes a necessary component of a comprehensive recovery program.
At Solace, we are dedicated to helping individuals reclaim their lives from the destructive effects of eating disorders. If you or a loved one are seeking treatment, we invite you to contact us for more information on our tailored treatment programs. Our compassionate team is always available to address any concerns you may have regarding eating disorders.